How Much Money Would Be Alotted For Mva Multiple Contusions
Abstract
Pulmonary contusion is a mutual finding after edgeless breast trauma. The physiologic consequences of alveolar hemorrhage and pulmonary parenchymal devastation typically manifest themselves within hours of injury and commonly resolve inside approximately vii days. Clinical symptoms, including respiratory distress with hypoxemia and hypercarbia, peak at about 72 h after injury. The timely diagnosis of pulmonary contusion requires a high degree of clinical suspicion when a patient presents with trauma caused by an appropriate mechanism of injury. The clinical diagnosis of acute parenchymal lung injury is unremarkably confirmed by thoracic computed tomography, which is both highly sensitive in identifying pulmonary contusion and highly predictive of the demand for subsequent mechanical ventilation. Management of pulmonary contusion is primarily supportive. Associated complications such every bit pneumonia, acute respiratory distress syndrome, and long-term pulmonary inability, withal, are frequent sequelae of these injuries.
Introduction
Pulmonary contusion is a mutual result of major trauma [one]. A review of data from the Trauma Registry at University Infirmary in San Antonio, TX indicated that 1722 (27%) of 6332 patients with multiple traumatic injuries and an Injury Severity Score (ISS) of 15 or higher had pulmonary contusions. Although thoracic injuries among children are uncommon, 50% of such lesions involve pulmonary contusion [2].
Amid civilian trauma populations, falls and rapid deceleration after vehicular crashes are the predominant mechanisms of lung injury. Recent reports from the Crash Injury Enquiry and Engineering Network (CIREN) [iii] demonstrated that two pregnant predictors of pulmonary contusion are an instantaneous modify in velocity (delta V) of more than 45 mph (odds ratio [OR] = 1.9) and a frontal crash into a fixed object (OR = 1.eight) [3]. Well-nigh-side lateral touch during a vehicular crash has as well been implicated as an important machinery leading to this lesion [3, iv]. In the combat setting, the shock wave produced by explosions and loftier-velocity projectiles may crusade serious trauma to the pulmonary parenchyma.
The clinical manifestations of lung injuries may be insidious; respiratory difficulty and radiographic findings may get evident hours subsequently injury. Patients who sustain pulmonary contusions are at a higher risk than other trauma patients of subsequent adverse events, including pneumonia and acute respiratory distress syndrome (ARDS), and long-term respiratory disability may result. Although for children the mechanism of injury differs from that for adults and generally involves being struck by a motor vehicle equally a pedestrian, the outcomes of pulmonary contusions appear to be like for both age groups [5]. Patients who take experienced trauma involving high-energy transfer should be evaluated for pulmonary contusion because prompt diagnosis and intervention may amend outcome.
History
The initial reports of pulmonary contusion focused on the description of severe lung injury with an "intact thorax" [6]. The kickoff description of pulmonary trauma without associated chest wall injury has been attributed to Morgagni in 1761; the initial commentary in the English medical literature was written by R. West. Smith of Dublin in 1840 [6]. In these early reports, the occurrence of serious lung injury in the absence of associated bony trauma was attributed to the elasticity of the chest wall of younger patients. As Laurent [7] commented in 1883, "A xvi-twelvemonth-old boy was injured when a wheel passed over his chest, when he fell while attempting to jump on a moving horse cart. At dissection, there was no external evidence of breast wall injury, but both lungs were severely contused with small lacerations. Beer was noted in the stomach!" With the exception of scattered example reports, nonetheless, little else was written well-nigh lung trauma until the beginning of the twentieth century.
In describing their experiences with injured soldiers from the battlefields of World War I, several authors reported that soldiers in proximity to the detonation of high explosives sometimes died equally a result of pulmonary complications. Initially, these deaths were attributed to a diversity of causes, including inhalation of toxic gases, sudden vacuum effect in gas-containing parts of the trunk, and fifty-fifty injury to the nervous system [8–10]. In 1918 and 1919, Hooker [11] conducted landmark studies by exposing animals to artillery blasts; these studies were the beginning to demonstrate that lung hemorrhage was responsible for the respiratory dysfunction observed after blast injuries. When state of war one time again bankrupt out in Europe in 1939, the World War I experiences were reviewed in apprehension of similar mechanisms of injury during Globe War Two. Reports from the Castilian Civil War and World War I described soldiers found dead on the battlefield with no credible external injury but with severe pulmonary hemorrhage at autopsy [12–14]. During the bombing of Britain in World War Two, both civilians and soldiers who were shut to explosions sustained severe "respiratory embarrassment" [xv–nineteen]. The prevalence of thoracic injuries during air raids prompted new investigations of blast-induced pulmonary injury.
At that time, considerable controversy existed as to whether the observed pulmonary pathology was due to the issue of suction (negative-force per unit area moving ridge) on the lungs, the excessive amplification of the lungs by air (positive-force per unit area moving ridge), or the straight impact of the blast on the chest wall itself. Zuckerman [20] conducted elegant experiments designed to determine the cause of lung injury in animals placed at various distances from explosive charges. He found that the most common lesion was pulmonary hemorrhage and that the severity of injury was directly related to the distance of the subject from the epicenter of the smash. A primal observation of his written report was that protective garments appeared to assist to lessen the severity of lung injuries acquired by boom mechanisms. This finding supported the theory that lung injury after explosive blasts is due primarily to the straight impact of the force per unit area moving ridge on the chest wall [20, 21]. Other investigators later on demonstrated that protective gear could also prevent lung injury after nail exposure in a submerged environment [22, 23].
Severe battleground lung injuries proved common during Globe War II [24]. Burford and Burbank [25] described the occurrence of "moisture lung" among Allied soldiers with chest injuries. These investigators examined 114 patients within 72 h of injury and found two distinct phenomena: the injured lung produced more interstitial and intra-alveolar fluid than the normal lung, and the injured lung appeared less able to rid itself of accumulated fluid. Burbank et al. [25, 26] attributed their findings to vigorous fluid resuscitation of patients who had experienced lung injury equally the result of thoracic trauma.
In contrast to descriptions of pulmonary contusion associated with military experiences, descriptions of pulmonary contusion related to civilian trauma were sparse before the 1960s. In 1965, Demuth [27] was amongst the first to suggest that pulmonary contusion was a common occurrence after noncombatant thoracic trauma. He reported pulmonary contusions in 47 patients, which constituted ten% of all thoracic injuries treated over a 10-twelvemonth catamenia in a rural area of Pennsylvania. With an increasing recognition of the incidence of this pulmonary lesion, investigators turned their attending to the institution of better diagnostic and predictive markers for pulmonary contusion. In 1965, Reid and Baird [28] reported their 2-year feel with 33 patients presenting with crushed breast injuries. They hypothesized that direct damage to the lung itself (rather than the associated bony injury) was the primary crusade of respiratory dysfunction, and they proposed that arterial blood gas measurements could be used to classify the severity of the resulting respiratory derangements.
By the stop of the 1960s, the typical pathophysiology and evidently radiographic findings associated with pulmonary contusion had been well delineated [28–31]. The experience of military machine surgeons during the Vietnam disharmonize provided farther details about the role of loftier-velocity missiles and blast injuries as causative mechanisms for pulmonary contusion. The apply by these surgeons of more than sophisticated laboratory and monitoring techniques [32–34] provided the foundation upon which most of today's management techniques for pulmonary contusion are based.
Pathophysiology and pathology
Clemedson [35] described the chief causes of pulmonary contusion subsequently Globe War II. Three basic phenomena appear to contribute to the incidence of these lung injuries. The kickoff is the spalling result, the shearing or bursting effect that tin can occur at the interface between a gas and a liquid (or betwixt other media with large differences in density). This phenomenon is visible when a shock wave from a depth charge reaches the surface of the sea, resulting in a "spray dome." When air-containing organs such as the lung are exposed to such forces, the spalling effect may result in the disruption of the alveolus at the signal of its initial contact with the shock wave. The second phenomenon is the inertial event that occurs when low-density alveolar tissue is stripped from heavier hilar tissues because the 2 types of tissue advance at different rates in response to the blast. The third phenomenon is the implosion effect that results from rebound or overexpansion of gas bubbling as pressure waves pass. In addition to these three bones effects, the pulmonary parenchyma may besides be torn past excessive amplification.
Air- and gas-containing portions of the body, such every bit the eardrums, the lungs, and the hollow viscera, are particularly vulnerable to the direct effects of blasts. The lungs may as well be injured as a result of interaction with the surrounding thoracic cage. The activity of external mechanical forces on the bony and cartilaginous outer structures can cause mechanical trigger-happy of lung tissue or directly laceration due to displacement of fractured ribs or chest wall compression. An example of blast issue on the lung occurred in 1967 when the destroyer Eliat was sunk by Egyptian missile boats near Port-Said. Sailors were apparently floating in the ocean when a 2d missile struck the sinking ship, injuring 32 of them. 19 men had both lung and bowel injuries, while eight had isolated pulmonary lesions [36].
Parenchymal lung injury leads to pathophysiologic changes, the severity of which depends on the extent of injury; it may as well lead to respiratory failure. Bleeding into uninvolved lung segments may crusade bronchospasm and may compromise alveolar function. Associated increases in the production of mucus, decreases in the clearance of fungus from the airways, and decreases in the production of surfactant by injured alveolar tissues may also contribute to pulmonary dysfunction [37].
Segmental lung damage can result in ventilation/perfusion mismatch, elevations in intrapulmonary shunt, increases in lung fluid, and loss of lung compliance [38]. These pathologic changes manifest themselves clinically in the form of hypoxemia, hypercarbia, and increased work of breathing [30]. Patients may present with rapid respiratory rate, rhonchi or wheezes, or even hemoptysis. Associated changes may not be visible on patently breast radiographs until 4–six h later injury, and these changes may non accurately reflect the extent to which the pulmonary tissue is affected [29]. In full general, the respiratory derangements associated with pulmonary contusions resolve within 3–v days, merely delayed deterioration may occur. Late pulmonary dysfunction may also occur after contusion as a consequence of the local inflammatory response to injury and sequestered blood, the systemic inflammatory responses related to associated injuries, or the development of nosocomial pneumonia [37].
Severe pulmonary hemorrhage, or "hepatization of the lung," was the typical anatomic finding in lung contusions examined by Hooker [11]. Pathologic findings at autopsy have revealed lesions characterized by lengthened hemorrhage: phrenicocostal sinus contusions with related liver damage, rib markings, massive hilar contusions, or hemorrhagic spots (Fig. 1) [18, 39]. Animal model studies accept identified a characteristic pattern of lesion progression after injury [xl, 41]. This progression is marked by initial interstitial hemorrhage, followed after 1–ii h past the onset of interstitial edema. These animal models have demonstrated that the architecture of the lung appears to exist preserved just that the infiltration of monocytes and neutrophils is credible at early intervals. At 24 h after injury, protein, red claret cells, and massive accumulations of inflammatory cells are found in the air spaces, along with fibrin and loss of normal architecture equally massive edema increases. By 48 h later injury, large amounts of fibrin and jail cell droppings and large numbers of type Two alveolar jail cell-derived granulocytes, neutrophils, and macrophages have accumulated. At this stage, the lymphatic vessels announced to be dilated and filled with protein. Past 7–10 days after traumatic lung injury, healing is almost consummate in these animals, with little balance scarring [42].
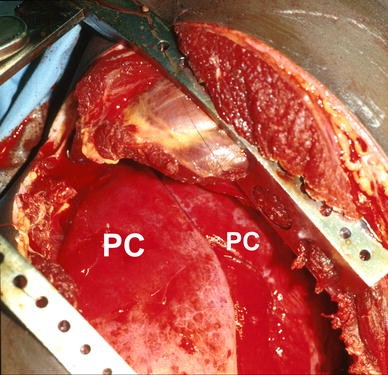
Gross anatomic pic of left hemithorax during emergency thoracotomy. Pulmonary contusion (PC) noted involving multiple lobes of the lung
Later pulmonary contusion, astute pathologic changes are associated with important physiologic alterations in hemodynamics [43]. Using computed tomography (CT) to determine the caste of injury and correlating this quantification with estimates of pulmonary vascular resistance and shunt fraction, investigators accept found that some patients experience serious pulmonary vasoconstriction later on injury. It has been postulated that this finding reflects a compensatory mechanism that limits perfusion to traumatized parenchyma, thereby minimizing any increase in shunt fraction. Some patients ("nonreactors") do not exhibit this response but instead, for unknown reasons, exhibit unchecked increases in shunt fraction [43].
Imaging
Early on reports of plain radiography findings associated with pulmonary contusion described characteristic consolidation patterns consistent with "traumatic pneumonia" (Fig. 2), typically actualization inside 4–vi h after injury [20, 44] and "vanishing" within a few days [45]. There appears to exist a relationship between the extent of abnormalities seen on chest radiograph and the severity of clinical findings [46–48]. In primate models of injury, the findings of breast radiography have been noted to underestimate the actual caste of injury as adamant at autopsy [49]. In the clinical setting, the exclusive utilise of plain chest radiographic imaging often contributes to the underdiagnosis of pulmonary contusion: only 47% of lesions are detected at the time of admission, whereas 92% are seen 24 h after injury [50]. In add-on, it should exist noted that enlargement of lung contusions on 10-ray during the first 24 h is mostly a negative prognostic sign. Furthermore, the caste of contusion can be hard to separate clinically from the effects of aspiration, fluid overload, transfusion (eastward.g., TRALI), and embolization. Interpretation of CT scan images can lead to confusion in differentiating pulmonary collapse/consolidation from aspiration with direct contusion, and hemothorax tin mimic intrapulmonary hemorrhage. Information technology should exist noted that the CT browse may place radiographic abnormalities that are deemed pulmonary contusions which exercise not lead to whatsoever respiratory dysfunction. These lesions therefore are of minimal clinical relevance and may exist deemed asymptomatic. Some authors have suggested therefore that the latest generation of CT scanners may be overly sensitive in delineating this lesion and that those patients with pulmonary contusion identified by "CT-merely" appear to have a better effect than those lung lesions noted on both plain radiographs and CT [51].
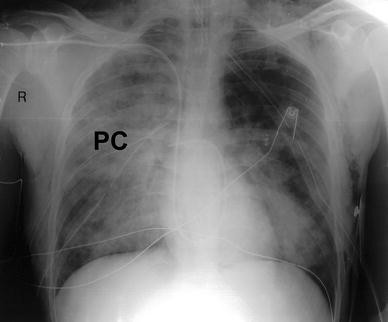
Chest radiograph demonstrating big pulmonary contusion (PC) involving correct lung
Attempts to use chest radiography findings to create scoring systems that can predict outcome after traumatic lung injury take been limited by the lack of sensitivity. Therefore, chest radiography findings accept been replaced in such scoring systems by thoracic CT findings (Fig. three), which accept proved highly authentic. A comparing of the findings of plain radiography and CT of the chest in a canis familiaris model establish that initial radiographs did non demonstrate the lesion in ii-thirds of the cases. In contrast, 100% of these lesions were discernable on initial CT scans. An assessment of clinical accuracy showed that radiographs obtained fifty-fifty vi h after injury failed to demonstrate pulmonary contusion in 21% of chest trauma patients. In improver, the findings of chest radiography contributed much more oft to the underestimation of the extent of lesions than did the findings of CT scans [52]. In a CT study of 103 patients with blunt thoracic trauma, 33 had pulmonary contusions that were not visible on a plain chest radiograph. A unique finding of chest CT scans is subpleural sparing, which can be seen in 95% of children with pulmonary contusion just is not seen in children with atelectasis or pneumonia [53]. Chest radiographs also grossly underestimate the caste of ventilation/perfusion mismatch, which can exist better estimated with nuclear imaging studies [54].
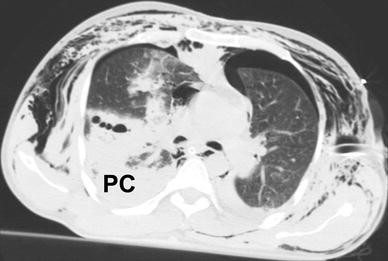
Thoracic CT browse demonstrating opacification representing pulmonary contusion (PC) of correct lung. Subcutaneous emphysema and pneumothoraces are seen bilaterally
Wagner et al. [55, 56] demonstrated that CT scans can effectively stratify pulmonary contusion injuries on the basis of the type and severity of the lesion. Using this nomenclature arrangement, the authors could predict the patient's need for ventilatory back up by determining the pct of airspace consolidation that was apparent on CT scans. When more than than 28% of the airspace was involved, all patients required subsequent mechanical ventilation. The ability of CT to discern the severity of pulmonary contusion has been confirmed by other investigators [57, 58]. Spiral CT allows the clinician to predict reliably which patients will feel astringent hypoxemia. Miller et al. [58] assessed 49 patients with pulmonary contusions (35 bilateral). The lesions were classified according to contusion volume as moderate (volume <twenty%; n = 32) or severe (book ≥20%; n = 17). The average contusion volume was 18% (range = five-55%). The moderate and severe groups were similar in ISS (moderate, 26.5; severe, 23.3; P = 0.33), admission blood pressure level (moderate, 129 mmHg; severe, 131 mmHg; P = 0.90), and the ratio of the arterial partial pressure of oxygen (PaOii) to the fraction of inspired oxygen (FiO2) at the time of admission (PaO2/FiO2; moderate, 255; severe, 197; P = 0.fourteen). Nonetheless, the charge per unit of ARDS in the moderate contusion group (22%) was much lower than that in the severe group (82%; P < 0.001).
Other investigators have found similar relationships between the corporeality of lung volume injured, equally demonstrated on CT scans, and the extent of pulmonary derangements [59]. Contemporary researchers have proposed the apply of magnetic resonance imaging [60], nuclear imaging [61], and even ultrasonography [62] for the diagnosis of pulmonary contusion. For example, some investigators have establish that breast ultrasonography, well known to be extremely user dependent, is highly sensitive and specific in diagnosing pulmonary contusion [63]. They support the use of this imaging method in both the emergency heart [63] and the intensive intendance unit of measurement (ICU) [64]. Considering of the high accuracy and reproducibility of CT and its ready availability at most trauma centers, this imaging technique is currently the standard of care for the diagnosis and adventure stratification of pulmonary contusions [56–58]. However, there may be no need to get a CT scan for a patient with a mild pulmonary contusion and no physiologic compromise.
Direction
Initial interventions
The direction of pulmonary contusion is primarily supportive. Beginning in the prehospital setting, supplemental oxygen and rapid assessment of airway and breathing should be undertaken as recommended by standard trauma protocols. Because pulmonary contusions may be associated with astringent hypoxemia, patient transport tin exist hazardous. During prehospital transfer, some of these patients may do good from being placed and then that the obviously injured hemothorax is in a dependent position; this positioning limits bleeding into the contralateral, less injured lung. Notwithstanding, such positioning may worsen hypoxemia considering the effect of gravity may increase blood period to the injured lung and cause a greater ventilation/perfusion mismatch.
After arriving at the hospital, the patient should be speedily examined and treated in accordance with modern principles of trauma care. Very rarely, patients with unilateral pulmonary contusions accompanied by massive intratracheal bleeding or severe air leaks may require early selective bronchial intubation [65]. Alternatively, patients with diffuse lung contusions may require endobronchial blockers, which accept been used successfully to command hemoptysis [66]. Bronchial blockers tin help control bleeding into the uninjured lung, provide tamponade at bleeding sites, and decrease the likelihood of air embolization. They eliminate the demand for the risky procedure of changing endotracheal tubes when a severely injured patient requires 1-lung or dual-ventilator management. The use of one-lung ventilation for a patient with unilateral thoracic injuries improves oxygenation and reduces the ventilation/perfusion mismatch while maintaining airway pressures within a condom range [67]. Rarely, dual-lung ventilation and fifty-fifty lobectomy may be needed for patients with very severe pulmonary injuries [68]. Severe hypoxemia or hemodynamic instability after pulmonary contusions may preclude the routine use of whole-body CT for trauma patients. In such circumstances, ultrasonography or diagnostic peritoneal lavage should be used to exclude intestinal injuries, and transesophageal echocardiography should be used to exclude aortic injuries.
Optimization of oxygenation and ventilation
Aggressive pulmonary toilet, meticulous fluid management, and control of chest wall pain are paramount in the treatment of all patients with pulmonary contusion. In cases of severe injury, intensive monitoring is besides essential for ensuring adequate organ perfusion and oxygenation. For patients with astringent unilateral lung lesions, arterial desaturation may exist minimized by the utilize of a kinetic or rotating bed [69]. Nosotros have observed that rotating patients with an uninjured contralateral hemithorax into the dependent position can meliorate oxygenation, possibly by increasing blood flow to the uninjured or "skilful" lung and optimizing the ventilation/perfusion relationship. The use of constantly rotating beds has been shown to significantly reduce the incidence of pneumonia and the number of ventilator days after major thoracic trauma [seventy]. If specialty rotating beds are not available, intermittent decumbent positioning (instituted past some authors for intervals totaling 8 h per day) [71] significantly increases oxygenation parameters later severe to moderate traumatic lung injury.
Patients should undergo intubation only if they showroom respiratory difficulties [72]. In addition, noninvasive positive-pressure ventilation (NPPV) may be appropriate for selected patients with pulmonary contusion and hypoxemia. Antonelli et al. [73] performed a prospective multicenter evaluation of ii,770 patients with hypoxemic acute respiratory failure. Of these, 354 met the criteria for NPPV and did not initially undergo intubation. Of the patients who underwent NPPV, seventy% did not require any intubation; the greatest success in avoiding intubation was observed in patients with cardiogenic pulmonary edema (90 of 99 patients, xc%) or pulmonary contusion (59 of 72 patients, 82%). Well-nigh 10% of patients with astute lung injury (ALI) (PaO2/FiO2 = 200-300) may avoid intubation if treated with NPPV [74].
Underlying pulmonary illness or associated injuries may dictate the demand for ventilatory support in certain patients. When required, mechanical ventilation strategies should exist tailored to optimize oxygenation while minimizing the potential for secondary lung injury. Several strategies have been used successfully, including those that accept emphasized the routine use of alveolar recruitment maneuvers [75] and permissive hypercapnia in difficult cases [76]. For patients with ALI or ARDS after pulmonary contusion, lung recruitment maneuvers (increasing intrinsic and extrinsic positive end-expiratory force per unit area [PEEP] to open previously closed lung units; using high-frequency inverse ratio ventilation) take been shown to increase arterial oxygenation, normally aerated lung volume, and total lung book while decreasing the amount of complanate lung tissue [75]. The successful utilize of high-frequency oscillatory ventilation for patients with severe pulmonary contusions has also been reported [77, 78].
Interestingly, direct harm to the lung after trauma alters the composition of surfactant. A report that used daily bronchial alveolar lavage to analyze unilateral pulmonary contusions in xviii patients found that full phospholipid concentrations and the percentage contents of phosphatidylcholine and sphingomyelin were significantly higher in the contused lungs than in the normal lungs [79]. Afterward, a small prospective randomized pilot study (northward = 8 per arm) found that adjunctive exogenous bovine surfactant replacement (single dose, 200 mg/kg) improved oxygenation and decreased ventilatory requirements in patients with pulmonary contusions and hypoxemia. [lxxx]. Any ventilation strategy or adjunctive therapy should optimize oxygenation while minimizing the risk of boosted ventilator-associated barotrauma [81]. When oxygenation is non possible, as may be the case for patients with ARDS afterwards pulmonary contusion in spite of the use of typical heroic measures (high-frequency ventilation, prone positioning, nitric oxide inhalation, prostaglandin infusion), extracorporeal membrane oxygenation (ECMO) has occasionally been life-saving [82].
Pain command and restoration of pulmonary mechanics
The pain associated with an injury to the thoracic wall may contribute substantially to hypoventilation in patients with pulmonary contusion. Aggressive attempts to alleviate discomfort and restore unhindered pulmonary mechanics are mandatory. Regional analgesia is preferred to establish pain command whenever possible as oral or intravenous medications alone typically do not successfully convalesce the astringent pain associated with rib fractures. Delay in alleviating chest wall pain may lead to hypoventilation, atelectasis, and subsequent respiratory deterioration. Intrapleural, paraspinal, or intercostal block may be a viable option, but the results of several studies suggest that epidural catheters provide optimal hurting relief and may improve outcome [83, 84]. Unfortunately, many trauma patients have spinal fractures or other injuries that preclude the utilise of epidural catheters. For example, Bulger et al. [83] studied 408 patients admitted with more three rib fractures. Of these, 282 (69%) met exclusion criteria, 80 could non consent, and 46 were prospectively randomly assigned to receive epidural hurting relief (due north = 22) or intravenous opioids (n = 24). The latter two groups were similar in mean age, injury severity score, sex, chest Abbreviated Injury Scale, and mean number of rib fractures. The epidural group had more flail segments (38 vs. 21%, P = 0.20) and pulmonary contusions (59 vs. 38%, P = 0.14) and required more breast tubes (95 vs. 71%, P = 0.03). However, in spite of this difference between groups in the number of direct pulmonary injuries, the rate of pneumonia was 18% for patients in the epidural group and 38% for patients in the intravenous opioid group. When the analysis was adjusted for direct pulmonary injury, the take chances of pneumonia was higher for the opioid group (OR = 6.0; 95% confidence interval [CI] = 1.0-35.0; P = 0.05). When the analysis was stratified for the presence of pulmonary contusion, the opioid group exhibited a twofold increase in the number of ventilator days required (incident rate ratio = 2.0; 95% CI = 1.6-ii.half-dozen; P < 0.001). Information technology therefore appears that a subset of patients with chest wall injury (approximately 1-third of severe chest wall injuries) are candidates for and benefit from epidural analgesia. The use of catheter-based commitment systems for continuous regional analgesia after thoracic surgery is an option that warrants boosted investigation [84].
Early experiences with operative chest wall fixation of flail breast in the setting of pulmonary contusions were not favorable [85]. However, the results of subsequent prospective investigations suggest that surgical stabilization may be beneficial in restoring chest wall mechanics and optimizing the subsequent ventilator course of patients with flail chest and pulmonary contusions. Tanaka et al. [86] prospectively compared the clinical effectiveness of surgical stabilization with that of routine ventilator direction in 37 patients with astringent flail chest injuries requiring prolonged ventilatory support. On twenty-four hours i after injury, patients were randomly assigned to surgical stabilization with Judet struts (northward = 18) or internal pneumatic stabilization (n = 19). The two groups were similar in ISS, chest Abbreviated Injury Score, number of rib fractures, severity of lung contusion, and PaO2/FIOtwo at the time of access. Compared to the routine care group, the surgical stabilization grouping experienced a shorter ventilatory period (10.eight ± 3.4 days vs. eighteen.3 ± 7.iv days), a shorter stay in the ICU (sixteen.five ± 7.4 days vs. 26.viii ± 13.2 days), and a lower incidence of pneumonia (24% vs. 77%); all differences were statistically significant at the level of P < 0.05. The number of patients who had returned to full-time employment by half dozen months after injury was also significantly higher in the surgical stabilization group (11 of xviii patients vs. 1 of 19 patients). These authors recommended surgical intervention for patients with severe flail chest injuries. Certainly, big prospective studies are required earlier routine use of rib plating can exist advocated.
Irrespective of the modality, an ambitious arroyo toward combating the furnishings of pain on pulmonary mechanics should be undertaken in all cases. Adequate pain control allows the critical intendance team to better institute chest physiotherapy and early on mobilization which are believed to assistance lower the likelihood of mechanical ventilation. Richardson et al. [87] found that aggressive critical care direction with such approaches for patients with severe chest trauma reduced the need for intubation from 100 to 23%, with an associated improvement in the survival rate from lx to 93.five%.
Resuscitation
Fluid management has been a controversial outcome since Burford and Burbank [25] attributed the incidence of "wet lung" in World War II soldiers with thoracic injuries to overzealous fluid administration. The results of studies using brute models have been inconclusive regarding the potential adverse effects of infused fluids [88–94], and relatively few man clinical trials accept addressed the impact of resuscitation on pulmonary contusion. Collins et al. [95] studied casualties from the Vietnam State of war and found that the volume of claret transfused was associated with the incidence of hypoxemia among soldiers who had sustained thoracic injuries, but but among those with evidence of straight lung trauma. A subsequent confirmatory report measured lung h2o in 16 civilian trauma patients presenting with shock (mean arterial pressure < 40 mmHg) and institute that lung h2o was increased only in the patients with pulmonary contusions, not in those with hemorrhagic shock in the absence of pulmonary trauma [96].
Other investigators, however, take plant no association between the amount of fluid resuscitation and the degree of pulmonary dysfunction or the need for ventilatory support later lung contusion [97, 98]. Later, compensatory pulmonary mechanisms such as increased lymph drainage in models of hemorrhagic stupor have been proposed as an explanation for many of the findings associated with the course of pulmonary contusion. Unfortunately, experimental information in this area have proved contradictory: some authors have found evidence of increased pulmonary capillary permeability (and increased lung water) in patients who accept undergone resuscitation for hemorrhagic shock [99], but others have non [100].
As our understanding of hemorrhagic shock continues to evolve, innovative resuscitative approaches have emerged. Hypertonic saline, for example, has been shown to finer restore perfusion after hemorrhagic shock, and the book requirement is smaller than that for traditional loftier-volume isotonic alternatives or blood production-based approaches [101]. The results of studies using beast models of hemorrhage suggested that the use of hypertonic saline, when compared to the utilise of isotonic fluids, may decrease the amount of edema in the brain [102] and the visceral organs [103, 104]. The results of studies using hypertonic saline in animal models of lung injury, however, have proved contradictory. Although some investigators accept found that hypertonic saline resuscitation for rats with pulmonary contusion decreases the amount of pulmonary inflammation and increases cellular protection [105], others have failed to detect whatsoever benefit [106]. In our serial of experiments using pigs subjected to pulmonary contusion and hemorrhage, small-volume hypertonic saline resuscitation failed to reduce the magnitude of lung injury or to provide substantial physiologic benefit over isotonic solutions [107]. No clinical studies have demonstrated a pulmonary physiologic benefit from the utilize of hypertonic saline subsequently thoracic injury. Recently, a big prospective trial evaluating the value of hypertonic saline resuscitation in trauma was terminated due to lack of credible efficacy (Eastward. Bulger, personal communication).
Scarlet blood cell substitutes, similar hypertonic saline, can restore perfusion afterward hemorrhagic shock fifty-fifty though limited fluid volumes are used [108]. Equally is true for hypertonic saline, however, the benefits of reddish blood cell substitutes for patients with thoracic injury have not been defined. Using a porcine model of pulmonary contusion and hemorrhage, nosotros [109] found that resuscitation with a hemoglobin-based blood substitute led to pulmonary hypertension, larger pulmonary contusions, and stiffer lungs.
Arginine vasopressin has emerged as a promising treatment offshoot for vasodilatory shock. Using a swine model, we [110] examined the therapeutic potential of administering vasopressin to animals subjected to astringent chest trauma and pulmonary contusion. Remarkably, the early use of vasopressin was associated with a decrease in the mortality charge per unit, a reduction in fluid requirements, and an comeback in pulmonary function. Clinical trials examining the effects of administering vasopressin specifically to trauma patients, including those with pulmonary contusion, are ongoing.
Antibiotics and steroids
No studies accept demonstrated a benefit from the rubber use of antibiotics afterward pulmonary contusion. Certainly, the indiscriminate apply of antimicrobial agents should be avoided so that the evolution of bacterial resistance can be limited. Similarly, no clinical findings suggest that corticosteroids are useful for patients with pulmonary contusion. The results of some animal studies suggest that steroid use may ameliorate hypoxemia and decrease the size of the contusion [111], but others have failed to find such benefits [112]. The use of steroids may, in fact, contribute to decreased bacterial clearance [94] and subsequent increases in the risk of pneumonia. It has been suggested that steroids decrease pulmonary vascular resistance subsequently injury, but the clinical do good of this event has not been established [113, 114]. Currently, corticosteroids have no role in the direction of pulmonary contusion.
Outcome
Overall outcomes after pulmonary contusion may be affected by the machinery and design of injury. Israeli investigators studied 154 patients who were injured equally a outcome of 17 bombing attacks; 28 (xviii.two%) of these patients sustained boom lung injuries. Patients with penetrating head injury and those with injuries to four or more trunk areas were significantly more likely to suffer from blast lung injury (OR = 3.47 and 4.12, respectively; P < 0.05) than were other victims of bombing attacks [115]. Experiences with civilian victims of blast injury suggest that although nigh patients with serious contusions due to this machinery of injury volition typically require mechanical ventilation, belatedly deterioration of pulmonary status is rare, expiry attributable to lung injury among those who survive the initial blast is unusual, and timely diagnosis and correct handling will produce splendid outcomes [116, 117].
The development of treat patients with pulmonary contusion has resulted in considerable improvement in outcomes. In spite of medical advances during the 1950s and 1960s, the utilize of ventilators, antibiotics, and monitoring failed to reduce the agin outcomes associated with pulmonary contusions. Historically, the mortality rate after these lung injuries was approximately 40% [27, 118, 119]. Although the utilise of ventilators markedly decreased the number of early deaths due to respiratory failure, it was associated with delayed mortality due to sepsis and with tracheostomy complications [120]. Before the 1970s, all patients with crushed chest injuries underwent mechanical ventilation. Trinkle et al. [72] were among the showtime to implement a selective intubation protocol for thoracic trauma patients with respiratory compromise. They reported that 427 patients with edgeless chest trauma underwent selective intubation, whereas 328 such patients were managed initially without intubation (only 10 of these patients eventually required ventilator support). The mortality rate in this study was 6.v%.
Pulmonary contusion does, however, increase the take a chance of morbidity for victims of trauma. The results of fauna and clinical studies support the notion that pulmonary contusion decreases the clearance of leaner [94] and predisposes patients to pulmonary infection [121]. For patients with astringent thoracic wall injury or flail chest, pulmonary parenchymal injury markedly increases both the likelihood of intubation (from twenty to fifty%) [87] and the associated bloodshed rate (from 16 to 42%) [122]. The severity of contusion predicts the need for ventilatory support after thoracic trauma [55]. Pulmonary contusion has been shown repeatedly to be an of import gamble factor for ARDS [123–125]. In ane early study, pulmonary contusion led to ARDS in 38% of l multitrauma patients [126]. A recent written report found that ARDS developed in 200 (five%) of 4397 patients with blunt trauma. The strongest predictors of the development of ARDS were an ISS higher than 25 (area under the receiver operating characteristic [ROC] curve, 0.72) and pulmonary contusion (surface area under the ROC curve, 0.68) [123]. Of annotation, intramedullary nailing of the femur or tibia does not announced to increase the chance of respiratory dysfunction for multitrauma patients with pulmonary contusions [127]. An interesting new imaging process, 18F-fluorodeoxyglucose positron emission tomography (FDG PET), has facilitated the determination of which patients with pulmonary contusions are likely to experience ARDS. The patients who later develop ARDS demonstrate lengthened FDG uptake, whereas other thoracic trauma patients with pulmonary contusions practise not [128].
Post-traumatic empyema is a rare but serious sequela of pulmonary contusion. In one study, empyema was found in merely 71 (3%) of 2261 thoracic trauma patients. The about important risk factors for empyema were retained hemothorax (OR = 5.50; P < 0.001) and pulmonary contusion (OR = iii.06; P < 0.001) [129].
The long-term consequences of pulmonary contusion have non been clearly defined. Kishikawa et al. [130] investigated the touch on of lung trauma on patients with flail chest who had (n = 12) or did not accept (n = ix) pulmonary contusion. Before discharge and six months after injury, patients underwent both spirometry and blood gas analysis. No balance pulmonary derangements were institute after flail chest alone, but persistent abnormalities in functional residue capacity (approaching endmost volume) and oxygenation were detected after lung contusion. Patients with pulmonary contusion, but not those with flail breast alone, oftentimes exhibited disabling dyspnea. Subsequent chest CT scans revealed fibrosis in the lungs of pulmonary contusion patients with dyspnea [130]. Leone et al. [131] performed long-term follow-upwardly on 55 patients with multiple trauma associated with edgeless chest trauma. Six months subsequently injury they noted that pulmonary function tests were impaired, and physical function was decreased in lxx% of patients, resulting in reduced pulmonary-specific quality of life. On the other hand, two Israeli studies institute that near patients with blast lung injury will either experience no long-term sequelae [97] or regain good role inside 12 months after injury [131]. 11 survivors of severe blast injury to the lung were examined 1 year after injury and were institute to have normal lung function and complete resolution of pulmonary parenchymal abnormalities, as shown past chest radiographs [132]. Among children with pulmonary contusion, long-term follow-up (iv.5 ± 1.0 years) revealed normal lung function and normal appearance on chest images [133].
Summary
Pulmonary contusion is common later on mechanisms of injury that impart substantial kinetic energy to the thorax. Hemorrhage into the lung substance leads to pulmonary pathophysiologic changes that worsen for 24–48 h and then generally resolve past seven days later injury. The diagnosis of pulmonary contusion is confirmed by pulmonary dysfunction and radiographic findings. Computed tomography of the chest is clearly superior to evidently radiography in identifying a pulmonary contusion and may exist helpful in predicting the need for mechanical ventilation and the likelihood of pneumonia or ARDS. Management of patients with pulmonary contusion is supportive and requires judicious fluid assistants, control of the hurting associated with bony thoracic injuries, and careful hemodynamic monitoring. In spite of before long available diagnostic and therapeutic interventions, pulmonary contusions are associated with substantial morbidity.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- CI:
-
Confidence interval
- CIREN:
-
Crash Injury Enquiry and Engineering science Network
- CT:
-
Computed tomography
- Delta V:
-
Change in velocity
- ECMO:
-
Extracorporeal membrane oxygenation
- FDG:
-
Fluorodeoxyglucose
- FIO2 :
-
Fraction of inspired oxygen
- ICU:
-
Intensive care unit
- ISS:
-
Injury Severity Score
- NPPV:
-
Noninvasive positive pressure ventilation
- OR:
-
Odds ratio
- PaO2 :
-
Arterial partial pressure of oxygen
- PEEP:
-
Positive terminate-expiratory pressure
- PET:
-
Positron emission tomography
- ROC:
-
curve Receiver operating characteristic curve
References
-
Cohn SM (1997) Pulmonary contusion: a review of a clinical entity. J Trauma 42:973–979
-
Balci AE, Kazez A, Eren Due south et al (2004) Blunt thoracic trauma in children: review of 137 cases. Eur J Cardiothorac Surg 26:387–392
-
O'Connor JV, Kufera JA, Kerns TJ et al (2009) Crash and occupant predictors of pulmonary contusion. J Trauma 66:1091–1095
-
Gayzik FS, Martin RS, Gabler HC et al (2009) Characterization of crash-induced thoracic loading resulting in pulmonary contusion. J Trauma 66:840–849
-
Allen GS, Cos CS Jr, Moore FA et al (1997) Pulmonary contusion: are children different? J Am Coll Surg 185:229–233
-
Fallon M (1940) Lung injury in the intact thorax with report of a instance. Br J Surg 28:39–49
-
Laurent EA (1883) Rupture of both lungs without external injury. Lancet two:457
-
Rex JD, Curtis GM (1942) Lung injury due to the detonation of loftier explosive. Surg Gynecol Obstet 74:53–62
-
Mott FW (1916) The effects of high explosives upon the central nervous system. Lancet 4824:333–338
-
Williams ERP (1942) Smash effects in warfare. Br J Surg 30:38–49
-
Hooker DR (1924) Physiological effects of air concussion. Am J Physiol 67:219–274
-
Lockwood AL (1940) Some experiences in the last state of war. Br Med J 1:356–358
-
Thomson FG (1940) Notes on penetrating chest wounds. Br Med J 1:44–46
-
Kretzschmar CH (1940) Wounds of the chest treated by bogus pneumothorax. Lancet 1:832–834
-
Dean DM, Thomas AR, Alison RS (1940) Effects of high-explosive boom on the lungs. Lancet two:224–226
-
Falla ST (1940) Effect of explosion-blast on the lungs. Br Med J 2:255–256
-
Hadfield G, Christie RV (1941) A case of pulmonary concussion ("nail") due to high explosive. Br Med J one:77–78
-
Barcroft J (1941) Lung injuries in air raids. Br Med J 1:239–242
-
Wilson JV (1943) Pathology of closed injuries of the breast. Br Med J 1:470–474
-
Zuckerman S (1940) Experimental written report of blast injuries to the lungs. Lancet 2:219–224
-
Desaga H (1950) Nail injuries. In: US Air Strength (ed) German aviation medicine, vol ii, Chap. XIV-D. Us Government Printing Function, Washington, DC, pp 1274–1293
-
Cameron GR, Short RHD, Wakeley CPG (1942) Pathological changes produced in animals past depth charges. Br J Surg 30:49–64
-
Clark SL, Ward JW (1943) The furnishings of rapid pinch waves on animals submerged in water. Surg Gynecol Obstet 77:403–412
-
Savage O (1945) Pulmonary concussion ("boom") in non-thoracic battle wounds. Lancet 248:424–429
-
Burford TH, Burbank B (1945) Traumatic wet lung. Observations on certain physiologic fundamentals of thoracic trauma. J Thorac Surg 14:415–424
-
Brewer LA, Burbank B, Samson PC (1946) The "wet lung" in state of war casualties. Ann Surg 123:343–362
-
Demuth Nosotros Jr, Smith JM (1965) Pulmonary contusion. Am J Surg 109:819–823
-
Reid JM, Baird WL (1965) Crushed breast injury: some physiological disturbances and their correction. Br Med J one:1105–1109
-
Alfano GS, Hale HW Jr (1965) Pulmonary contusion. J Trauma 5:647–658
-
Garzon AA, Seltzer B, Karlson KE (1968) Physiopathology of crushed chest injuries. Ann Surg 168:128–136
-
Fulton RL, Peter ET, Wilson JN (1970) The pathophysiology and treatment of pulmonary contusions. J Trauma 10:719–730
-
Moseley RV, Doty DB, Pruitt BA Jr (1969) Physiologic changes post-obit chest injury in combat casualties. Surg Gynecol Obstet 129:233–242
-
Lichtmann MW (1970) The problem of contused lungs. J Trauma 10:731–739
-
Ratliff JL, Fletcher JR, Kopriva CJ et al (1971) Pulmonary contusion: a continuing management problem. J Thorac Cardiovasc Surg 62:638–644
-
Clemedson CJ (1956) Blast injury. Physiol Rev 36:336–354
-
Huller T, Bazini Y (1970) Blast injuries of the breast and abdomen. Arch Surg 100:24–30
-
Demling RH, Pomfret EA (1993) Blunt chest trauma. New Horiz one:402–421
-
Oppenheimer L, Chicken KD, Forkert L et al (1979) Pathophysiology of pulmonary contusion in dogs. J Appl Physiol 47:718–728
-
O'Reilly JN, Gloyne SR (1941) Boom injury of the lungs. Lancet 2:423
-
Fulton RL, Peter ET (1970) The progressive nature of pulmonary contusion. Surgery 67:499–506
-
Casley-Smith JR, Eckert P, Földi-Börcsök E (1976) The fine construction of pulmonary contusion and the effect of various drugs. Br J Exp Pathol 57:487–496
-
Moseley RV, Vernick JJ, Doty DB (1970) Response to blunt chest injury: a new experimental model. J Trauma 10:673–683
-
Wagner RB, Slivko B, Jamieson PM et al (1991) Consequence of lung contusion on pulmonary hemodynamics. Ann Thorac Surg 52(ane):51–57
-
Westermark N (1941) A roentgenological investigation into traumatic lung changes arisen through blunt violence to the thorax. Acta Radiol 22:331–346
-
Williams JR (1959) The vanishing lung tumor: pulmonary hematoma. Am J Roentgenol Radium Ther Nucl Med 81:296–302
-
Stevens E, Templeton AW (1965) Traumatic nonpenetrating lung contusion. Radiology 85:247–252
-
Rodriguez RM, Hendey GW, Marek 1000 et al (2006) A pilot study to derive clinical variables for selective chest radiography in blunt trauma patients. Ann Emerg Med 47(five):415–418
-
Tyburski JG, Collinge JD, Wilson RF et al (1999) Pulmonary contusions: quantifying the lesions on breast X-ray films and the factors affecting prognosis. J Trauma 46(five):833–838
-
Erickson DR, Shinozaki T, Beekman E et al (1971) Human relationship of arterial blood gases and pulmonary radiographs to the degree of pulmonary damage in experimental pulmonary contusion. J Trauma 11:689–694
-
Pape HC, Remmers D, Rice J et al (2000) Appraisement of early evaluation of blunt breast trauma: development of a standardized scoring organization for initial clinical conclusion making. J Trauma 49:496–504
-
Deunk J, Poels T, Brink K et al (2010) The clinical event of occult pulmonary contusion on multidector-row computed tomography in blunt trauma patients. J Trauma 68:387–394
-
Schild HH, Strunk H, Wever W et al (1989) Pulmonary contusion: CT vs evidently radiograms. J Comput Assist Tomogr 13:417–420
-
Donnelly LF, Klosterman LA (1977) Subpleural sparing: a CT finding of lung contusion in children. Radiology 204:385–387
-
Van Eeden SF, Klopper JF, Alheit B et al (1989) Ventilation-perfusion imaging in evaluating regional lung function in nonpenetrating injury to the breast. Breast 95:632–638
-
Wagner RB, Jamieson PM (1989) Pulmonary contusion. Evaluation and nomenclature by computed tomography. Surg Clin Due north Am 69:31–xl
-
Wagner RB, Crawford WO Jr, Schimpf PP (1988) Classification of parenchymal injuries of the lung. Radiology 167:77–82
-
Gayzik FS, Hoth JJ, Daly M et al (2007) A finite element-based injury metric for pulmonary contusion: investigation of candidate metrics through correlation with computed tomography. Stapp Car Crash J 51:189–209
-
Miller PR, Croce MA, Bee TK et al (2001) ARDS after pulmonary contusion: accurate measurement of contusion volume identifies high-risk patients. J Trauma 51:223–228
-
Mizushima Y, Hiraide A, Shimazu T et al (2000) Changes in contused lung book and oxygenation in patients with pulmonary parenchymal injury after blunt breast trauma. Am J Emerg Med xviii(four):385–389
-
Weishaupt D, Hilfiker PR, Schmidt Thou et al (1999) Pulmonary hemorrhage: imaging with a new magnetic resonance claret pool amanuensis in conjunction with breathheld three-dimensional magnetic resonance angiography. Cardiovasc Intervent Radiol 22:321–325
-
Esme H, Kaya Eastward, Solak O et al (2007) Using 99mTc-DPTA radioaerosol inhalation lung browse as compared with computed tomography to detect lung injury in blunt breast trauma. Ann Nucl Med 21:393–398
-
Brawl CG, Ranson MK, Rodriguez-Galvez M et al (2009) Sonographic delineation of posttraumatic alveolar-interstitial disease: the hand-held diagnosis of a pulmonary contusion. J Trauma 66:962
-
Soldati G, Testa A, Silva FR et al (2006) Chest ultrasonography in lung contusion. Chest 130:533–538
-
Rocco Yard, Carbone I, Morelli A et al (2008) Diagnostic accuracy of bedside ultrasonography in the ICU: feasibility of detecting pulmonary effusion and lung contusion in patients on respiratory support after severe blunt thoracic trauma. Acta Anaesthesiol Scand 52:776–784
-
Inoue H, Suzuki I, Iwasaki Thou et al (1993) Selective exclusion of the injured lung. J Trauma 34:496–498
-
Nishiumi N, Nakagawa T, Masuda R et al (2008) Endobronchial haemorrhage associated with blunt chest trauma treated by bronchial occlusion with a Univent. Ann Thorac Surg 85:245–250
-
Cinnella Yard, Dambrosio Grand, Brienza N et al (2001) Contained lung ventilation in patients with unilateral pulmonary contusion. Monitoring with compliance and EtCO(two). Intensive Care Med 27:1860–1867
-
Zandstra DF, Stoutenbeek CP (1988) Monitoring differential CO2 excretion during differential lung ventilation in disproportionate pulmonary contusion. Clinical implications. Intensive Intendance Med 14:106–109
-
Hasan FM, Beller TA, Sobonya RE et al (1982) Effect of positive end-expiratory pressure level and body position in unilateral lung injury. J Appl Physiol 52:147–154
-
Fink MP, Helsmoortel CM, Stein KL et al (1990) The efficacy of an oscillating bed in the prevention of lower respiratory tract infection in critically ill victims of edgeless trauma. A prospective report. Chest 97:132–137
-
Voggenreiter G, Neudeck F, Aufmkolk 1000 et al (1999) Intermittent prone positioning in the handling of severe and moderate posttraumatic lung injury. Crit Care Med 27:2375–2382
-
Trinkle JK, Richardson JD, Franz JL et al (1975) Management of flail chest without mechanical ventilation. Ann Thorac Surg xix:355–363
-
Antonelli Chiliad, Conti G, Moro ML et al (2001) Predictors of failure of noninvasive positive pressure level ventilation in patients with astute hypoxemic respiratory failure: a multi-heart study. Intensive Care Med 27:1718–1728
-
Vidhani K, Kause J, Parr M (2002) Should we follow ATLS guidelines for the management of traumatic pulmonary contusion: the function of not-invasive ventilatory support. Resuscitation 52:265–268
-
Schreiter D, Reske A, Stichert B et al (2004) Alveolar recruitment in combination with sufficient positive end-expiratory force per unit area increases oxygenation and lung aeration in patients with severe chest trauma. Crit Care Med 32:968–975
-
Sorkine P, Szold O, Kluger Y et al (1998) Permissive hypercapnia ventilation in patients with severe pulmonary blast injury. J Trauma 45:35–38
-
Funk DJ, Lujan East, Moretti EW et al (2008) A brief study: the use of loftier-frequency oscillatory ventilation for severe pulmonary contusion. J Trauma 65:390–395
-
Shapiro MJ, Keegan MJ (1992) Continuous oscillation therapy for the treatment of pulmonary contusion. Am Surg 58:546–550
-
Aufmkolk M, Fischer R, Voggenreiter G et al (1999) Local consequence of lung contusion on lung surfactant composition in multiple trauma patients. Crit Care Med 27:1441–1446
-
Tsangaris I, Galiatsou Eastward, Kostanti Eastward et al (2007) The effect of exogenous surfactant in patient with lung contusions and acute lung injury. Intensive Care Med 33:851–855
-
[No authors listed] (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for astute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 342:1301–1308
-
Madershahian N, Wittwer T, Strauch J et al (2007) Application of ECMO in multitrauma patients with ARDS as rescue therapy. J Card Surg 22:180–184
-
Bulger EM, Edwards T, Klotz P et al (2004) Epidural analgesia improves effect after multiple rib fractures. Surgery 136:426–430
-
Luchette FA, Radafshar SM, Kaiser R et al (1994) Prospective evaluation of epidural versus intrapleural catheters for analgesia in chest wall trauma. J Trauma 36:865–870
-
Voggenreiter G, Neudeck F, Aufmkolk M et al (1998) Operative breast wall stabilization in flail chest–outcomes of patients with or without pulmonary contusion. J Am Coll Surg 187:130–138
-
Tanaka H, Yukioka T, Yamaguti Y et al (2002) Surgical stabilization or internal pneumatic stabilization? A prospective randomized study of management of severe flail breast patients. J Trauma 52:727–732
-
Richardson JD, Adams 50, Flint LM (1982) Selective management of flail chest and pulmonary contusion. Ann Surg 196:481–487
-
Daniel RA Jr, Cate WR Jr (1948) "Wet lung": an experimental study: I. The effects of trauma and hypoxia. Ann Surg 127:836–857
-
Rutherford RB, Valenta J (1971) An experimental study of "traumatic wet lung". J Trauma 11:146–166
-
Trinkle JK, Furman RW, Hinshaw MA et al (1973) Pulmonary contusion. Ann Thorac Surg xvi:568–573
-
Fulton RL, Peter ET (1973) Physiologic effects of fluid therapy after pulmonary contusion. Am J Surg 126:773–777
-
Fulton RL, Peter ET (1974) Compositional and histologic furnishings of fluid therapy post-obit pulmonary contusion. J Trauma xiv:783–790
-
Richardson JD, Franz JL, Grover FL et al (1974) Pulmonary contusion and hemorrhage: crystalloid versus colloid replacement. J Surg Res sixteen:330–336
-
Richardson JD, Woods D, Johanson WG Jr et al (1979) Lung bacterial clearance post-obit pulmonary contusion. Surgery 86:730–735
-
Collins JA, James PM, Bredenberg CE et al (1978) The relationship between transfusion and hypoxemia in combat casualties. Ann Surg 188:513–520
-
Tranbaugh RF, Elings VB, Christensen J (1982) Determinants of pulmonary interstitial fluid accumulation after trauma. J Trauma 22:820–826
-
Bongard FS, Lewis FR (1984) Crystalloid resuscitation of patients with pulmonary contusion. Am J Surg 148:145–151
-
Johnson JA, Cogbill Thursday, Winga ER (1986) Determinants of result after pulmonary contusion. J Trauma 26:695–697
-
Michel RP, Laforte Yard, Hogg JC (1981) Physiology and morphology of pulmonary microvascular injury with shock and reinfusion. J Appl Physiol 50:1227–1235
-
Demling RH, Niehaus G, Will JA (1979) Pulmonary microvascular response to hemorrhagic shock, resuscitation, and recovery. J Appl Physiol 46:498–503
-
Velasco Information technology, Pontieri V, Rocha east Silva M Jr et al (1980) Hyperosmotic NaCl and severe hemorrhagic shock. Am J Physiol 239:H664–H673
-
Wisner DH, Schuster 50, Quinn C (1990) Hypertonic saline resuscitation of caput injury: effects on cerebral water content. J Trauma 30:75–78
-
Toung TJ, Nyquist P, Mirski MA (2008) Effect of hypertonic saline concentration on cerebral and visceral organ h2o in an uninjured rodent model. Crit Care Med 36:256–261
-
Toung TJ, Chen CH, Lin C et al (2007) Osmotherapy with hypertonic saline attenuates water content in encephalon and extracerebral organs. Crit Care Med 35:526–531
-
Fernandes TR, Pontieri 5, Moretti AI et al (2007) Hypertonic saline solution increases the expression of oestrus shock poly peptide 70 and improves lung inflammation early after reperfusion in a rodent model of controlled hemorrhage. Shock 27:172–178
-
Roch A, Blayac D, Ramiara P et al (2007) Comparison of lung injury later on normal or small volume optimized resuscitation in a model of hemorrhagic shock. Intensive Care Med 33:1645–1654
-
Cohn SM, Fisher BT, Rosenfield AT et al (1997) Resuscitation of pulmonary contusion: hypertonic saline is not beneficial. Shock 8:292–299
-
Schultz SC, Hamilton IN Jr, Malcolm DS (1993) Use of base deficit to compare resuscitation with lactated Ringer's solution, Haemaccel, whole blood, and diaspirin cross-linked hemoglobin post-obit hemorrhage in rats. J Trauma 35:619–625
-
Cohn SM, Zieg PM, Rosenfield AT (1997) Resuscitation of pulmonary contusion: effects of a ruby-red cell substitute. Crit Care Med 25:484–491
-
Feinstein AJ, Cohn SM, King DR et al (2005) Early vasopressin improves short-term survival after pulmonary contusion. J Trauma 59:876–883
-
Franz JL, Richardson JD, Grover FL et al (1974) Effect of methylprednisolone sodium succinate on experimental pulmonary contusion. J Thorac Cardiovasc Surg 68:842–844
-
Shepard GH, Ferguson JL, Foster JH (1969) Pulmonary contusion. Ann Thorac Surg 7:110–119
-
Svennevig JL, Bugge-Asperheim B, Vaage J et al (1984) Corticosteroids in the treatment of blunt injury of the chest. Br J Blow Surg xvi:lxxx–84
-
Svennevig JL, Bugge-Asperheim B, Bjørgo S et al (1980) Methylprednisolone in the treatment of lung contusion following blunt chest trauma. Scan J Thorac Cardiovasc Surg fourteen:301–305
-
Almogy G, Mintz Y, Zamir 1000 et al (2006) Suicide bombing attacks: tin can external signs predict internal injuries? Ann Surg 243:541–546
-
Avidan V, Hersch M, Armon Y et al (2005) Blast lung injury: clinical manifestations, handling, and effect. Am J Surg 190:927–931
-
Pizov R, Oppenheim-Eden A, Matot I et al (1999) Blast injury from an explosion on a civilian bus. Breast 115:165–172
-
Relihan G, Litwin MS (1973) Morbidity and mortality associated with flail breast injury: a review of 85 cases. J Trauma 13:663–671
-
Keller JW, Meckstroth CV, Sanzenbacher 50 et al (1967) Thoracic injuries due to blunt trauma. J Trauma 7:541–550
-
Ransdell HT Jr (1965) Handling of flail chest injuries with a piston respirator. J Trauma 5:412–420
-
Freedland M, Wilson RF, Bough JS et al (1990) The direction of flail chest injury: factors affecting outcome. J Trauma xxx:1460–1468
-
Clark GC, Schecter WP, Trunkey DD (1988) Variables affecting event in blunt chest trauma: flail breast vs. pulmonary contusion. J Trauma 28:298–304
-
Miller PR, Croce MA, Kilgo PD et al (2002) Astute respiratory distress syndrome in blunt trauma: identification of independent gamble factors. Am Surg 68:845–850
-
Guo-shou Z, Xiang-jun B, Cheng-ye Z (2007) Analysis of high take a chance factors related to acute respiratory distress syndrome following astringent thoracoabdominal injuries. Chin J Traumatol 10:275–278
-
Wu J, Sheng 50, Ma Y et al (2008) The assay of risk factors of impacting mortality rate in severe multiple trauma patients with posttraumatic acute respiratory distress syndrome. Am J Emerg Med 26:419–424
-
Pepe PE, Potkin RT, Reus DH et al (1982) Clinical predictors of the adult respiratory distress syndrome. Am J Surg 144:124–130
-
Handolin L, Pajarinen J, Lassus J et al (2004) Early intramedullary nailing of lower extremity fracture and respiratory part in polytraumatized patients with a breast injury: a retrospective report of 61 patients. Acta Orthop Scand 75:477–480
-
Rodrigues RS, Miller PR, Bozza FA et al (2008) FDG-PET in patients at risk for acute respiratory distress syndrome: a preliminary report. Intensive Care Med 34:2273–2278
-
Eren S, Esme H, Sehitoguillari A et al (2008) The risk factors and management of posttraumatic empyema in trauma patients. Injury 39:44–49
-
Kishikawa M, Yoshioka T, Shimazu T et al (1991) Pulmonary contusion causes long-term respiratory dysfunction with decreased functional residual chapters. J Trauma 31:1203–1208
-
Leone M, Bregeon F, Antonini F et al (2008) Long-term outcome in breast trauma. Anesthesiology 109:864–871
-
Hirschberg B, Oppenheim-Eden A, Pizov R et al (1999) Recovery from blast lung injury: 1-year follow-upward. Breast 116:1683–1688
-
Haxhija EQ, Nöres H, Schober P et al (2004) Lung contusion-lacerations after blunt thoracic trauma in children. Pediatr Surg Int 20:412–414
Acknowledgments
The authors recognize the fantabulous support provided by Catherine Hornsby, MBA, and Flo Witte, PhD, ELS, in manuscript preparation.
Writer information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cohn, S.Yard., DuBose, J.J. Pulmonary Contusion: An Update on Contempo Advances in Clinical Management. World J Surg 34, 1959–1970 (2010). https://doi.org/10.1007/s00268-010-0599-ix
-
Published:
-
Event Engagement:
-
DOI : https://doi.org/10.1007/s00268-010-0599-9
Keywords
- Lung Injury
- Acute Respiratory Distress Syndrome
- Injury Severity Score
- Hypertonic Saline
- Blunt Chest Trauma
Source: https://link.springer.com/article/10.1007/s00268-010-0599-9
Posted by: hornerthome1952.blogspot.com

0 Response to "How Much Money Would Be Alotted For Mva Multiple Contusions"
Post a Comment